Introduction
The NHS is under increasing pressure to deliver safe, high-quality care with fewer resources while supporting the wellbeing of a workforce at risk of burnout.
National policy, including the NHS 10-Point Plan to improve 1 doctors’ working lives, sets clear expectations for Trusts: reduce agency spend, ensure fulfilment of annual leave requests, eliminate payroll errors, and provide genuine flexibility through self-rostering.
The GMC National 2 Training Survey (2025) reinforces these priorities, showing that doctors with input into rota design report better work–life balance, while lack of flexibility and notice remain key concerns.
Across the UK, NHS departments using HealthRota have reported substantial reductions in agency spend, fulfilment of every annual leave request, elimination of payroll errors, and the ability for doctors to design their own rotas through self-rostering – outcomes that have historically been among the hardest to deliver and are at the heart of national workforce ambitions.
In this case study, we demonstrate how digital workforce transformation using HealthRota can turn these national policy ambitions into practical outcomes across NHS Trusts.
The Fiscal Impact
The BMA Medical Staffing Report (2021) warned that rota gaps and inefficiencies were driving unnecessary costs and fuelling reliance 4 on agency staff.
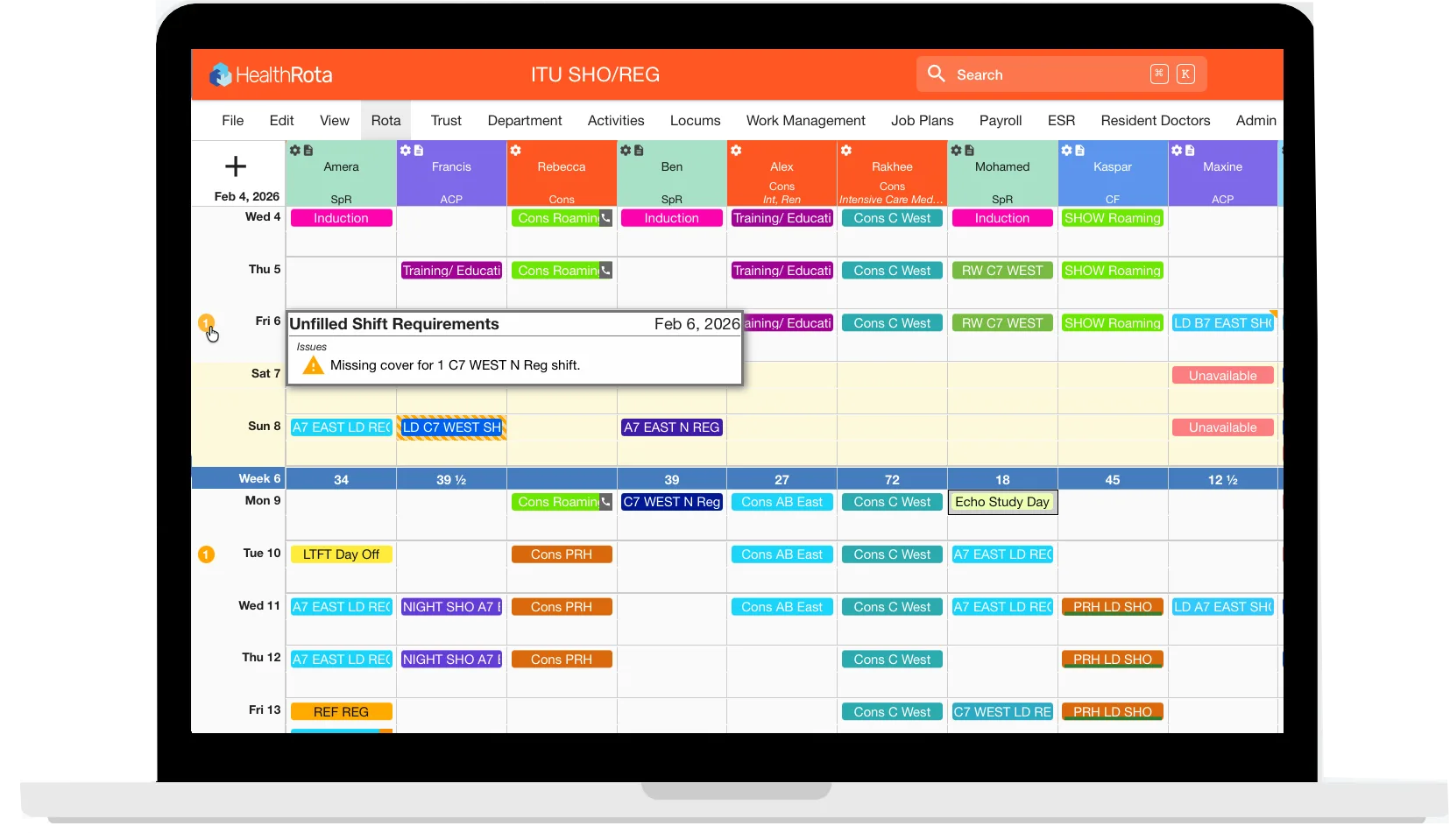
Research in BMJ Open (2022) reinforced this by linking poor rota design to inefficiency, attrition, and wasted resources. HealthRota addresses these pressures by enabling Trusts to define their exact coverage requirements and roster into those needs — ensuring optimal use of available staff, minimising rota gaps, and embedding compliance and transparency to unlock savings.
At Hillingdon Hospitals, the paediatric department reduced rota creation from several days to hours, and saved thousands through reduced agency use. As Paediatric Registrar, Dr Sabrina Waheed, noted: “We saved nearly £16,000 for the department in just four months… it’s massive for something as simple as self-rostering” (Hillingdon Podcast, 2024).
Emergency medicine teams at Northern General Hospital in Sheffield also reported clear financial and operational benefits through real-time oversight of staffing levels, the reduction of last-minute locum bookings, and time savings for rota administrators.
At Leeds General Infirmary, HealthRota allowed the Emergency Department to more than double its consultant workforce, while reducing the administrative burden.
Consultant rota administration time fell by 77%, even with a 2.4x increase in the consultant workforce (18 > 44 consultants). Monthly rota creation time also dropped by 78% (4–5 days > 1 day), enabling senior clinicians to redirect valuable time back into education, supervision, and clinical care.
The finance team at University Hospitals Sussex NHS Foundation Trust used HealthRota to improve payroll forecasting and strengthen financial governance. Real-time workforce data enabled the Trust to allocate resources more effectively, reduce errors, and achieve better value for money.
These results demonstrate how HealthRota not only creates savings but also contributes to system-wide financial resilience. By reducing agency reliance, cutting administrative overheads, and enabling accurate financial planning, HealthRota supports the NHS goal of delivering more with less while protecting frontline care.

Safety and Risk Improvements
Patient safety is dependent on safe staffing, yet the reality for many doctors continues to involve long hours, missed breaks, and high levels of exception reporting.
Studies in the BMJ Open and the Emergency Medicine Journal (2023) 10 found that poor rota design is closely associated with fatigue, burnout, and compromised care. The GMC National Training Survey reinforced these risks, reporting that lack of flexibility and input into rota design remain among the most pressing concerns for doctors in training.
In the paediatric department at Bristol Royal Hospital for Children, where self-rostering was implemented in 2022 across all resident doctors, the Trust recorded significant improvements in wellbeing, rest, and work–life balance.
Resident doctors received 100% of their annual and study leave requests, compared with just 27% previously, and every respondent said they wanted to continue working in a department that self-rosters. Doctors also reported being more willing to pick up locum shifts as a result of greater flexibility and fairness in the rota design.
Meanwhile, registrars at Hillingdon used self- rostering to eliminate rota breaches caused by less-than-full-time trainees, ensuring compliance with the European Working Time Directive while also reducing sickness absence.
The scale of transformation is clearest at University Hospitals Sussex, where HealthRota has been rolled out for all medics across emergency, acute, and general medicine. Real-time visibility of staffing levels supports CQC inspections and board-level reporting, while enabling the Trust to proactively demonstrate compliance and manage workforce pressures.
HealthRota has transformed how we manage rotas across University Hospitals Sussex, giving doctors greater flexibility and control through annualised and self-preferencing rotas. With 83% of resident doctors and almost half of consultants now fully e-rostered, we’re creating a pan-trust model that’s fair, transparent, and future-ready.
Amy Brown, Medical Workforce Systems
Manager at University Hospitals Sussex
These departmental results align with findings from Professor Rob Galloway (see video below), which highlighted how HealthRota has improved compliance, reduced risk, and supported safer staffing across multiple hospital settings.
Annualised rotas and self-rostering/self-preferencing has created an equal distribution of shifts, reducing levels of burnout and ensuring that doctors only work the hours that they are paid for.
Wellbeing and Human Benefits
The NHS People Plan highlights flexible, inclusive working as a priority for staff retention. The GMC National Training Survey reinforces this, showing that autonomy in rota design is closely associated with improved work–life balance, while inflexibility and poor notice of changes remain widespread sources of dissatisfaction.
Broader research confirms the link; the Journal of Clinical Nursing (2023) found that inadequate rota planning increases stress and undermines retention.
Clinicians at Hillingdon gave powerful testimony to the impact of self-rostering. Dr Sabrina Waheed reflected: “It’s amazing the difference it can make to both staff morale and burnout. With the survey we did, registrars are happier. Happier staff mean better care for patients. ”
Her colleague, Dr Anna Burford, added: “We noticed a massive decrease in sickness on the registrar rota, because people are just more flexible”
Following the success of the registrar rota, the approach has already been extended to SHOs, underlining its scalability across grades.
In Bristol, self-rostering has significantly improved training opportunities for resident doctors. The system released extra capacity from the out-of-hours rota and increased normal working days by 38 days per full-time equivalent registrar – a 72% increase.
In-hours training time rose from 57% to 70% (23% rise), meeting RCPCH training targets, while Supporting Professional Activity (SPA) time covering teaching, training, and audit, increased to 16.5 hours per month, in line with the RCPCH Trainee Charter.
In addition to these educational benefits, the initiative also delivered measurable cost savings for the department.
The impact of HealthRota at Bristol Royal Hospital for Children
Self-rostering with HealthRota has revolutionised the way we build resident doctor rotas. We sought to rebalance the scales between training and service provision, putting resident wellbeing and training opportunities at the forefront. We demonstrated improved training quality and wellbeing while delivering significant financial savings. Our model could easily be applied to other settings and marks a step-change in our practice.
Dr Karthik Darma, Consultant Paediatrician & Workforce Planning Lead at Bristol Royal Hospital for Children
Doctors in Sussex highlighted the value of being able to swap shifts and book leave easily. Staff described this as a practical change that made a significant difference to their sense of control – directly reflecting the NHS ambition for “flexible working for all.”
Setting a New Benchmark
HealthRota is redefining rota management across the NHS by delivering measurable improvements in rota fairness, flexibility, compliance, and cost-efficiency.
These experiences demonstrate how HealthRota addresses not only the administrative burden of rota management but also the deeper human factors that determine whether NHS staff feel valued, supported, and able to thrive.
This is exactly the kind of change called for in the NHS; transparent, data-driven systems that protect staff, improve retention, and deliver value for patients.
By embedding these principles into the design of HealthRota, NHS Trusts are moving beyond reactive rota management to strategic workforce planning that is compliant, efficient, and resilient. The result is safer patient care, stronger financial stewardship, and a healthier and supported NHS workforce.